Studies
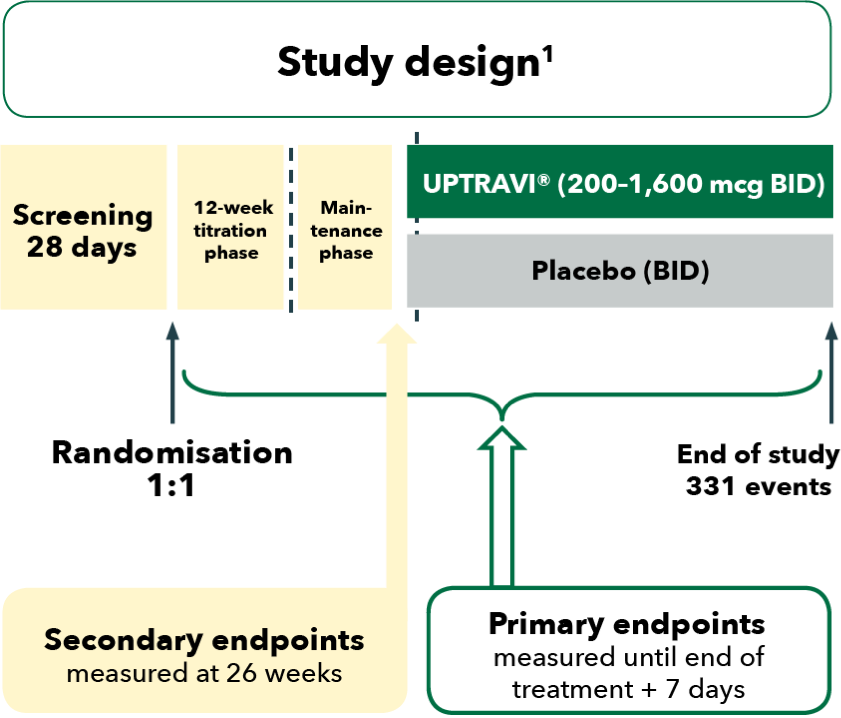
The safety and efficacy of UPTRAVI® were investigated in GRIPHON, a Phase 3 study assessing the long-term benefits of UPTRAVI® in pulmonary arterial hypertension (PAH) patients. The primary endpoint in GRIPHON was a composite of the time to the first morbidity or mortality event up to end of treatment.[1]
The GRIPHON study was a multicentre, double-blind, placebo-controlled, event-driven Phase 3 trial.[1]
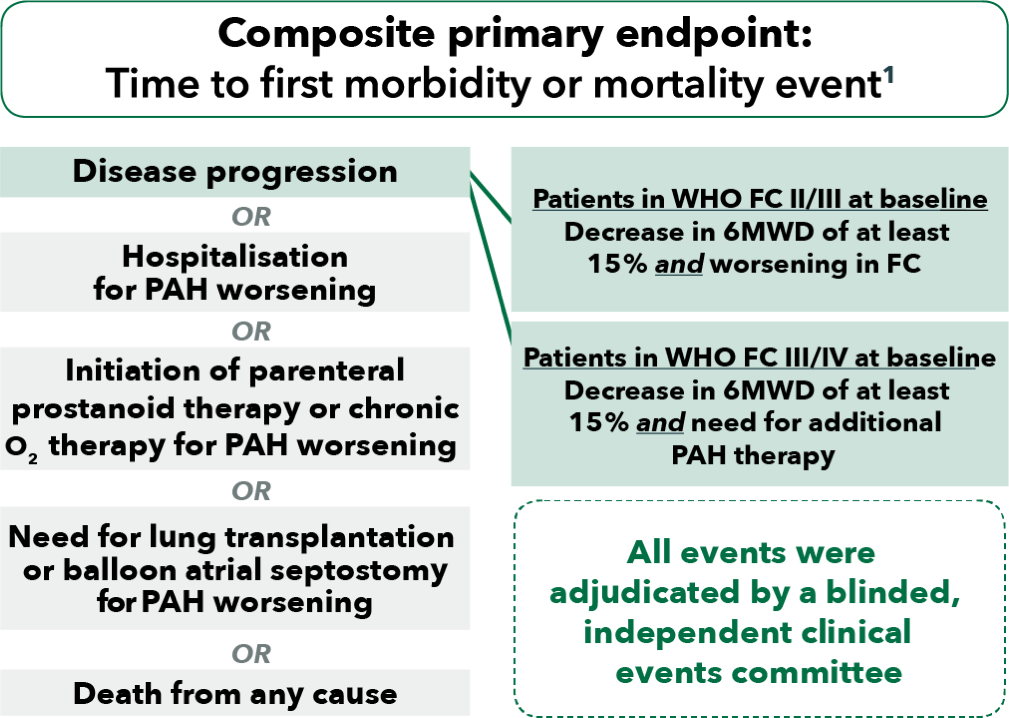
BID, twice daily; FC, functional class; PAH, pulmonary arterial hypertension; 6MWD, 6-minute walk distance; WHO, World Health Organization
The GRIPHON study assessed the safety and efficacy of UPTRAVI® across a broad range of patients with PAH.[1]
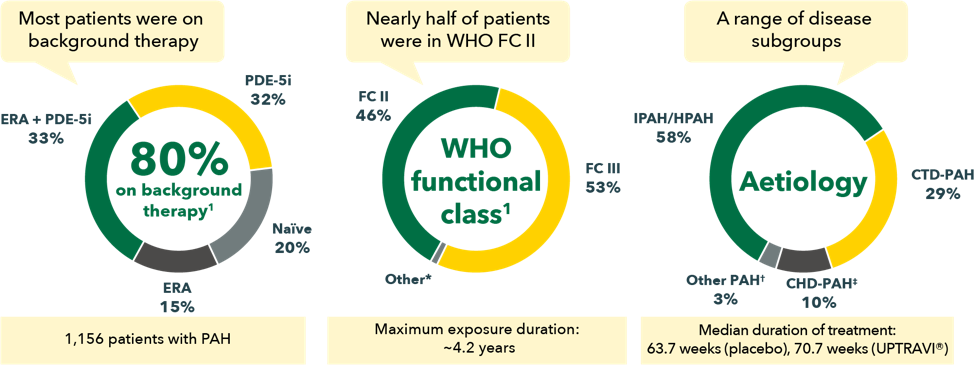
CHD, congenital heart disease; CTD, connective tissue disease; ERA, endothelin receptor antagonist; FC, functional class; HIV, human immunodeficiency virus; HPAH, heritable pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; PAH, pulmonary arterial hypertension; PDE-5i, phosphodiesterase type-5 inhibitor; WHO, World Health Organization
*9 patients were in FC I, 11 patients in FC IV.
†Other aetiologies included drug- or toxin-induced PAH (2%) and HIV-PAH (1%).
‡Patients with repaired congenital systemic-to-pulmonary shunts.
Evidence for the long-term efficacy of UPTRAVI® is based on GRIPHON primary endpoint data showing a 40% reduction of the risk of morbidity-mortality* vs placebo. The treatment effect of UPTRAVI® was consistent across prespecified subgroups, including aetiology and as monotherapy, in combination with an ERA or a PDE-5 inhibitor, or triple combination with both an ERA and a PDE-5 inhibitor.[1][2][3][4]
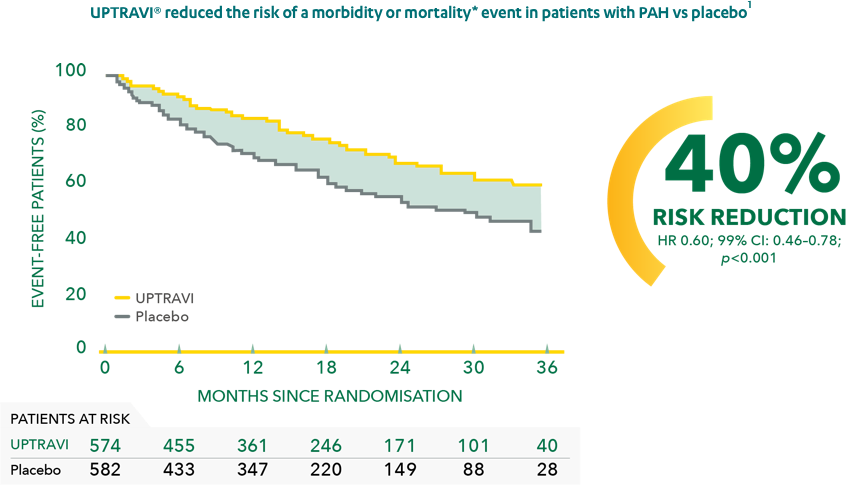
Adapted from Sitbon et al. 2015[1]>
CI, confidence interval; ERA, endothelin receptor antagonist; HR, hazard ratio; PAH, pulmonary arterial hypertension; PDE-5, phosphodiesterase type 5
*As measured by a composite primary morbidity-mortality endpoint. Results were driven by a decrease in disease progression and hospitalisations due to PAH; they do not apply to mortality on its own.
Consistent with the primary endpoint in the overall population, UPTRAVI® reduced the risk of a morbidity-mortality event* vs placebo in patients with CHD-PAH† by 42% (HR 0.58; 95% CI: 0.25–1.37)[2] and in patients with CTD-PAH by 41% (HR 0.59; 95% CI : 0.41–0.85).‡[3]
The treatment effect with UPTRAVI® was consistent in patients with CTD-PAH across the CTD subtypes. Compared with placebo, UPTRAVI® reduced the risk of morbidity-mortality* by 44% in patients with SSc-PAH, by 34% in patients with SLE-PAH and by 32% in patients with MCTD-PAH/other-CTD-PAH.[3]
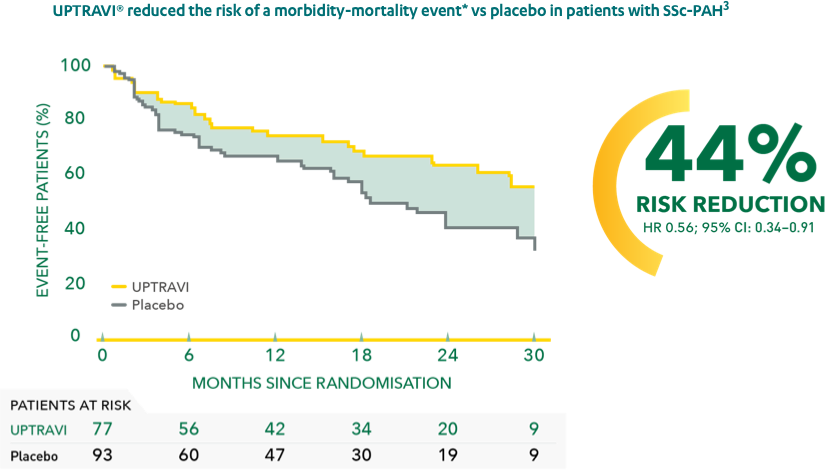
Adapted from Gaine et al. 2017[3]
CHD, congenital heart disease; CI, confidence interval; CTD, connective tissue disease; HR, hazard ratio; MCTD, mixed connective tissue disease; PAH, pulmonary arterial hypertension; SLE, systemic lupus erythematosus; SSc, systemic sclerosis
*As measured by a composite primary morbidity-mortality endpoint. Results were driven by a decrease in disease progression and hospitalisations due to PAH; they do not apply to mortality on its own.
†Patients with repaired congenital systemic-to-pulmonary shunts.
‡Patients with MCTD-PAH and other-CTD-PAH (HR 0.68; 95% CI: 0.31–1.47).
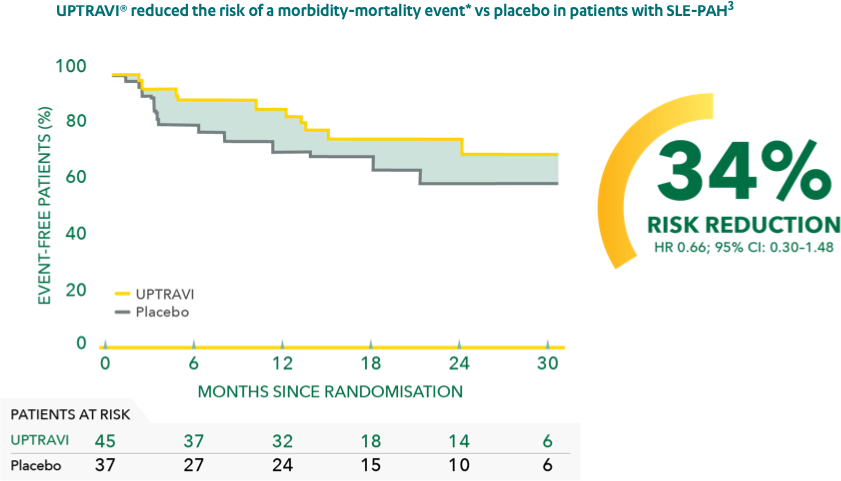
Adapted from Gaine et al. 2017[3]
CI, confidence interval; HR, hazard ratio; PAH, pulmonary arterial hypertension; SLE, systemic lupus erythematosus
*As measured by a composite primary morbidity-mortality endpoint . Results were driven by a decrease in disease progression and hospitalisations due to PAH; they do not apply to mortality on its own.
UPTRAVI® reduced the risk of morbidity-mortality* vs placebo by 37% in patients receiving double oral combination therapy with an ERA and a PDE-5i.[4]
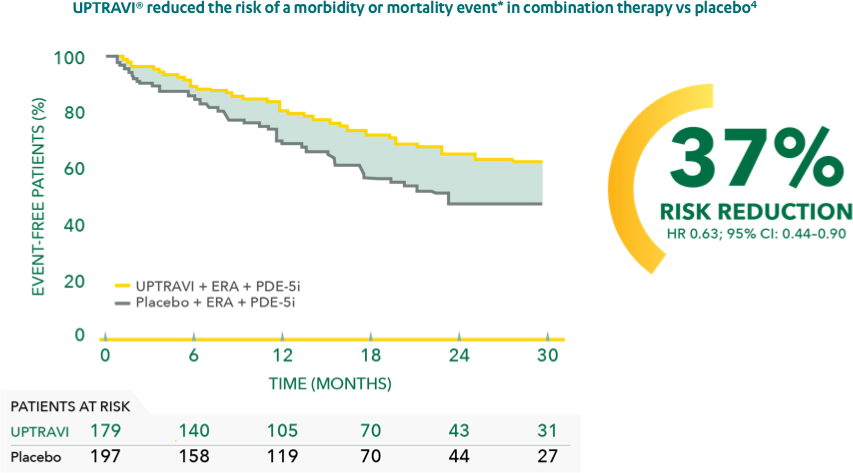
Adapted from Coghlan et al. 2018[4]
CI, confidence interval; ERA, endothelin receptor antagonist; HR, hazard ratio; PAH, pulmonary arterial hypertension; PDE-5i, phosphodiesterase type-5 inhibitor
*As measured by a composite primary morbidity-mortality endpoint. Results were driven by a decrease in disease progression and hospitalisations due to PAH; they do not apply to mortality on its own.
The effect of UPTRAVI® was consistent with the primary endpoint for all background therapy subgroups. UPTRAVI® reduced the risk of morbidity-mortality* vs placebo by 43% in patients not receiving any therapy at baseline (HR 0.57; 99% CI: 0.32–1.03; p=0.0068), by 42% in patients receiving PDE-5i monotherapy at baseline (HR 0.58; 99% CI: 0.37–0.91; p=0.0008) and by 34% in patients receiving ERA monotherapy at baseline (HR 0.66; 99% CI: 0.32–1.35; p=0.655).[5]
Addition of UPTRAVI® to double oral combination therapy reduced the risk of a morbidity-mortality event* in WHO FC II and FC III patients. The benefit of adding UPTRAVI® was seen early and was sustained throughout the long term.[4]
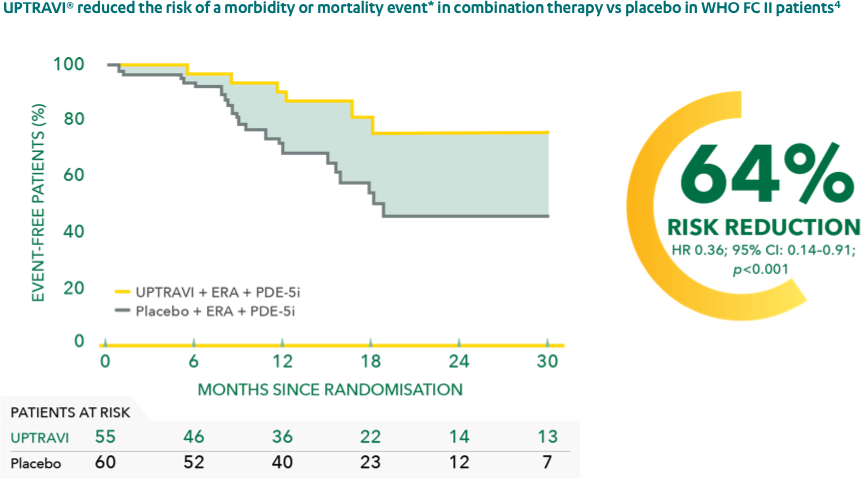
Adapted from Coghlan et al. 2018[4]
CI, confidence interval; ERA, endothelin receptor antagonist; FC, functional class; HR, hazard ratio; PAH, pulmonary arterial hypertension; PDE-5i, phosphodiesterase type-5 inhibitor; WHO, World Health Organization
*As measured by a composite primary morbidity-mortality endpoint. Results were driven by a decrease in disease progression and hospitalisations due to PAH; they do not apply to mortality on its own.
When added to double combination therapy, UPTRAVI® reduced the risk of morbidity-mortality* vs placebo by 26% in WHO FC III patients (HR 0.74; 95% CI: 0.50–1.10).[4]
UPTRAVI® demonstrated a 5-year survival estimate of over 75% in the open-label extension of the GRIPHON study.[6]
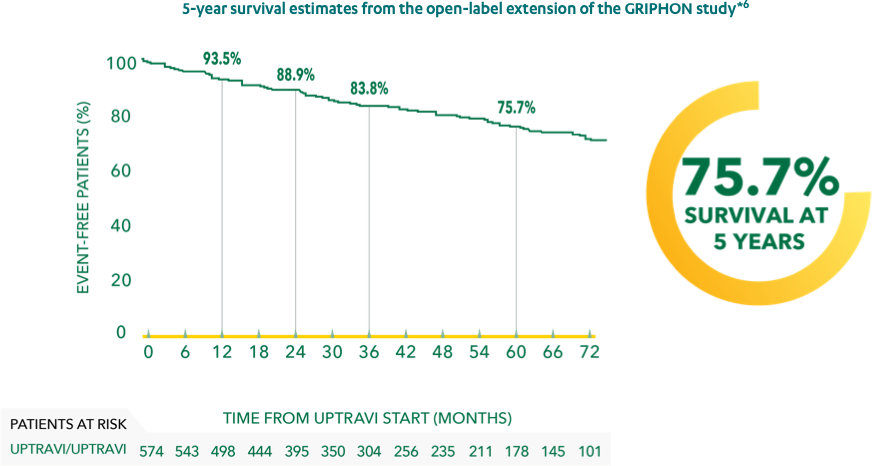
Adapted from Galiè et al. 2018[6]
*330 patients continuing on UPTRAVI® in the open-label extension after being randomised to UPTRAVI® in GRIPHON.
Learn More About UPTRAVI®
Patient Management
Advice on how to manage your UPTRAVI® patients, including details on dosage and side effects.
Guidelines
Details from the 2022 ESC/ERS guidelines to help you achieve and/or maintain a low-risk status for your patients with PAH.
